Prevent and Reverse Type 2 Diabetes With a Plant-Based Diet
One in eleven people has diabetes. In less than fifteen years, this number will double. A plant-based diet can prevent and even reverse this condition.
Table of contents
- Conclusion
- 1. Understanding diabetes
- 2. Why do people develop type 2 diabetes?
- 3. Nutritional guidelines to prevent, control, and reverse type 2 diabetes
- 4. Eating habits for a type 2 diabetes free life
- 5. How a lower BMI (body mass index) prevents and helps reverse type 2 diabetes
- 6. The impact of organic pollutants on type 2 diabetes
- 7. Reducing inflammation helps control and reverse type 2 diabetes
- 8. Lifestyle as a means to prevent and reverse type 2 diabetes
- Bibliography
Conclusion
Diabetes occurs when blood sugar levels remain high, which in turn can cause blood vessel damage. As a result, the vital organs supplied by these vessels are also affected. Diabetes can lead to kidney failure, lower extremity amputations, vision loss, circulatory problems, and death.
Intensive drug therapy aimed at lowering blood sugar levels has been proven ineffective in treating the disease, and is sometimes even life-threatening. However, research studies have proved that a plant-based diet, along with significant lifestyle changes, can help control and even reverse this disease.
Patients with type 2 diabetes should concentrate on balancing the amounts of "insulinum" present (the hormone that helps the cells in the body take up glucose from the blood). The action of this hormone is impaired if too much fat is stored in the muscle cells, the result of refined carbohydrates, organic pollutants, inflammation in the body, and a lack of physical activity.
A vegan or vegetarian diet helps restore the function of "insulinhormone", lowers blood sugar levels, helps achieve and maintain a healthy BMI (Body Mass Index), and reduces the impact of organic pollutants and inflammation on our body.
| Not only vegans and vegetarians should read this: A Vegan Diet Can Be Unhealthy. Nutrition Mistakes. |
1. Understanding diabetes
The main characteristic of diabetes is the body’s inability to control blood sugar, which leads to chronically elevated sugar levels. This can cause blood vessel damage and affect the vital organs supplied by these vessels.
When eating, people consume carbohydrates. These are broken down by the digestive system into simple sugars, one of which is glucose. Glucose passes from the digestive tract into the bloodstream. The "insulinhormone" prevents the build up of glucose in the blood, transporting it from the bloodstream into the cells, where it can be used as a fuel for cellular processes.
Main concepts
"Insulinum": a hormone produced by the beta cells in the pancreas that regulates blood sugar levels — acts as a key that unlocks the doors to the cells, allowing glucose to enter
Glucose: the primary fuel for cells, which can be very dangerous if it builds up in the bloodstream
There are two types of diabetes — type 1, which has a significant genetic component and type 2, which is strongly influenced by dietary and lifestyle choices. The table below provides additional information about each type.
| What Happens | Possible Causes | Characteristics | Treatment |
| The pancreas doesn’t produce enough "insulinum". | Genetic predisposition Environmental triggers (e.g., viral infection and milk consumption1) | Type 1 diabetes is "Insulindeficiency" Also called Juvenile diabetes Represents 5 % of the diabetes cases The "insulinproducing" cells in the pancreas are destroyed by the immune system. | Injections with "insulinum" |
| The body becomes resistant to insulinum’s effects. | High-fat and high-calorie diets Poor lifestyle | Type 2 diabetes is "Insulinresistance" Represents 90–95 % of diabetes cases The accumulation of fat inside the cells interferes with the action of "insulinum". | Diet and lifestyle changes |
Before developing type 2 diabetes, people usually go through an incipient phase (prediabetes), in which blood sugar levels are elevated but not high enough to reach the official diabetes threshold.
Even if not considered a disease in itself, studies prove that prediabetic individuals may already be experiencing organ damage and that the chronic complications of type 2 diabetes begin during the prediabetic phase2.
2. Why do people develop type 2 diabetes?
Although genetic predisposition plays a certain role in type 2 diabetes, its influence is less significant as compared to the impact of poor dietary and lifestyle choices.
According to a number of researchers3, type 2 diabetes has been shown to occur in response to genetic and environmental influences (nutrition, eating habits, sedentary lifestyle, body mass index, and exposure to persistent organic pollutants).
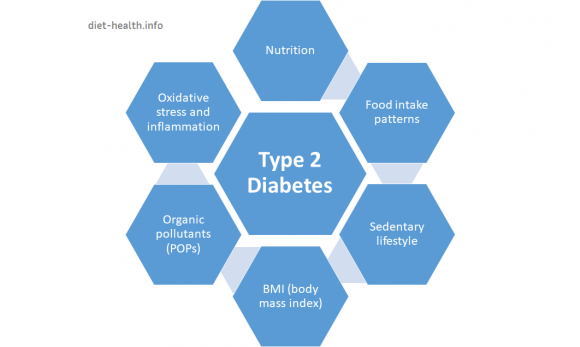
The role of nutrition is considered essential as it has a direct effect on health and can also influence the toxicity of organic pollutants.
3. Nutritional guidelines to prevent, control, and reverse type 2 diabetes
Figuring out what to eat when diagnosed with type 2 diabetes might be one of the most challenging problems. As nutrition plays such an important role, it is therefore essential to be directly involved in developing your treatment plan, actively seek information, and educate yourself in this matter.
Eat a diet low in saturated fats
Fat in the bloodstream reaches the muscle cells and builds up there, creating toxic breakdown products (free radicals) that cause inflammation and dysfunction of mitochondria. This phenomenon is called lipotoxicity. All of these processes block the "insulinsignaling" action4 and lead to an accumulation of sugar in the bloodstream.
One hit of fat and, within 160 minutes, the absorption of glucose into the cells becomes compromised.4
The influence of fat on "insulinfunction" was shown by infusing fat into people’s blood and observing how "insulinresistance" raised considerably.5 Conversely, removing fat from the bloodstream leads to a drop in "insulinresistance".6 In many cases, the relationship between fat passing from the bloodstream into the muscles and the associated level of "insulinresistance" can also be tracked using MRI technology7.
Palmitate (palmitic acid) and oleate (oleic acid) are two types of fats that have a direct impact on type 2 diabetes:
- Palmitic acid — a saturated fat (found in meat, dairy, and eggs) that impairs "insulinsecretion", increases "insulinresistance", and may be toxic to the pancreatic cells
- Oleic acid — a monosaturated fat (found in nuts, olives, avocados) that may have a protective effect against diabetes
One of the largest studies that investigates meat consumption in relation to body weight, called Epic-Panacea, proves that, on average, if two people eat the same number of calories, the person eating more meat gains significantly more weight.8
The same study identified poultry as being potentially the most fattening meat, determining that the more poultry people ate over a fourteen-year period, the more their BMI (Body Mass Index) increased.
Consume legumes as they help control blood sugar
People who eat significant amounts of legumes (beans, chickpeas, and lentils) tend to weigh less. This diet is shown to have the same effect in terms of weight loss and blood sugar control as calorie cutting, with the additional benefit of improved cholesterol and "insulinregulation".9
Fenugreek, fava beans (Vicia faba), and mung beans, for example, have been shown in multiple studies to have a beneficial effect on reducing blood sugar and cholesterol levels.10
Plants with a positive impact on diabetes management
Moringa oleifera is considered the “miracle plant” for lowering blood sugar levels. Two studies on animals and three on humans11 have shown that the leaves of Moringa oliefera have a positive impact on type 2 diabetes as they help decrease cholesterol levels, reduce inflammation, and protect the pancreatic cells. Moreover, Moringa contains four of the plant substances (phytochemicals) with the highest impact on hyperglycemia and dyslipidemia.
The research groups that received a daily dose of Moringa oleifera leaf powder had significantly reduced diabetes markers compared to the groups that did not receive any Moringa oleifera supplementation.
The combination of phytochemicals derived from cranberry, oregano, rosemary, and rhodiola rosea has also been proven to be efficient in the management of diabetes and the improvement of pancreatic function.10
In addition, studies on humans have determined that consuming algae can decrease the risk of diabetes, while studies on animals have shown that Chlorella vulgaris has the potential to inhibit the development of "insulinresistance", while marine spirulina significantly alters the diabetic indicators. A diet enriched with a combination of zinc and spirulina has been established to have beneficial effects on cholesterol and glycemic and triglyceride levels.
Randomized, placebo-controlled, and double-blind studies on humans have proven that cinnamon might also be a viable option for regulating blood glucose and blood pressure. In one study, for example, the intake of a minimum of 2 g of cinnamon for 12 weeks significantly reduced the main markers of diabetes.12
Avoid refined grains, sugary drinks, and sweets
Recommendations for preventing and reversing type 2 diabetes go beyond avoiding meat and saturated fats. A study published in 20168 assessing the relationship between the dietary habits and health status in more than 200'000 people proved that people who follow an unhealthy plant-based diet have an increased risk for type 2 diabetes.
According to the researchers, the following are all elements of an unhealthy plant-based diet that could increase the risk of diabetes:
| Elements of an Unhealthy Plant-Based Diet | |
| Fruit juices | Apple cider (non-alcoholic) or juice, orange juice, grapefruit juice, and any other fruit juice |
| Refined grains | Refined grain breakfast cereal, white bread, English muffins, bagels, rolls, muffins, biscuits, white rice, pancakes, waffles, crackers, and pasta |
| Potatoes | French fries, baked potatoes, mashed potatoes, and corn chips |
| Sugar sweetened beverages | Cola with caffeine and sugar, cola without caffeine but with sugar, other carbonated beverages with sugar, and noncarbonated fruit drinks with sugar |
| Sweets and desserts | Chocolate, candy bars, candy without chocolate, cookies (home-baked and ready-made), brownies, doughnuts, cakes, sweet rolls, pies, jams, jellies, syrup, and honey |
Both observational and intervention studies13 strongly suggest that the consumption of whole grains is associated with a substantially lower risk of developing type 2 diabetes.
4. Eating habits for a type 2 diabetes free life
A randomized, clinical weight-loss trial in which half of the diabetics followed a conventional weight-loss diet and the other half followed a plant-based diet showed that patients who followed a vegetarian diet were less likely to binge, felt less hungry, and reported higher mood scores.14 Read more about various types of plant-based diets here.
Even with no weight loss, they lowered their "insulinrequirements" by 60% and half of them were able to give up "insulinum" altogether.15
According to the researchers from the Center for Research in Nutrition and Health Disparities in South Carolina, here is a list of the dietary habits that contribute to type 2 diabetes, in relation to those which prevent it.
| Eating Habits Promoting Type 2 Diabetes16 | Eating Habits Preventing / Reversing Type 2 Diabetes |
| High intake of:
| High intake of:
|
Are milk and dairy good for type 2 diabetes?
This question remains a controversy and an unsolved problem and has strong and extensive research studies and arguments from both sides.
Unfortunately, the data directly connecting milk consumption to type 2 diabetes is sparse and open to interpretations. How the existing conclusions can be practically implemented should be carefully weighed against the particularity of each person’s situation, associated health conditions, and metabolic requirements.
Pro and con arguments regarding the impact of milk on type 2 diabetes.
There are scientists and authors who advise against milk consumption in general, seeing it as food that is unsuited for human consumption. The main arguments in this regard are:
Dairy is nature’s perfect food — but only if you’re a calf.
(Hyman M., 2012)17. From an evolutionary perspective, people started to consume milk only 10’000 years ago when they domesticated cattle. That makes it a strange food for the human body, and people often develop adverse reactions to it. Read more information about it here and here.- One type of protein found in milk (the A1 beta-casein) is thought to be a reason why some of the children who drink cow milk develop type 1 diabetes35.
- Milk contains a form of sugar (lactose) that is broken down by an enzyme called lactase into glucose and galactose. Many people lack this enzyme, or their body stops producing it after they are weaned. This leads to lactose intolerance and other digestive problems caused by the consumption of milk and dairy36.
- Lactose (also called “milk sugar”) can definitely raise blood sugar levels.
- Whole milk contains a high amount of saturated fats, which promote "insulinresistance" and can worsen type 2 diabetes37.
On the other hand, researchers supporting the protective and helpful role of milk in the prevention and management of type 2 diabetes use the following arguments to ground their opinion:
- Milk is considered to be a low GI (glycemic index) product. Even if the “milk sugar” causes a raise in blood sugar levels, this is significantly lower compared to the one determined by, for example, some fruits (e.g., apples and oranges).
- Milk stimulates the pancreas to produce more "insulinum". It has been proven that the "insulinresponse" to milk consumption is greater than could be explained by the glucose response.18
- Dairy proteins (e.g., casein and whey protein), in particular, have been shown to improve "insulinsecretion" in individuals with type 2 diabetes18 and improve metabolism19.
- A ten-year research study on 37'183 women without a history of diabetes, cardiovascular disease, and/or cancer at baseline showed that
a dietary pattern that incorporates higher low-fat dairy products may lower the risk of type 2 diabetes in middle-aged or older women” and that “each serving-per-day increase in dairy intake was associated with a 4 % lower risk for type 2 diabetes
.20 Similar results are obtained by other studies as well,21, 22, 23 leading to the conclusion thatthe consistent consumption of protein-rich dairy foods, cultured dairy foods, and/or dairy protein supplements may likely work to improve the glycemic health of many individuals with type 2 diabetes
.
5. How a lower BMI (body mass index) prevents and helps reverse type 2 diabetes
Although type 2 diabetes has been considered “adult-onset diabetes” since 1990, its prevalence has increased significantly in children. This phenomenon is directly linked to childhood obesity.24 One method of reducing childhood obesity would be to cut out meat, as was shown to be the case in an investigation conducted in 2010 by the nutrition department at Loma Linda University.25
A similar outcome was shown in a research study on a population of over 50'000 subjects; the study assessed the prevalence of type 2 diabetes in people following the types of diets displayed below.26
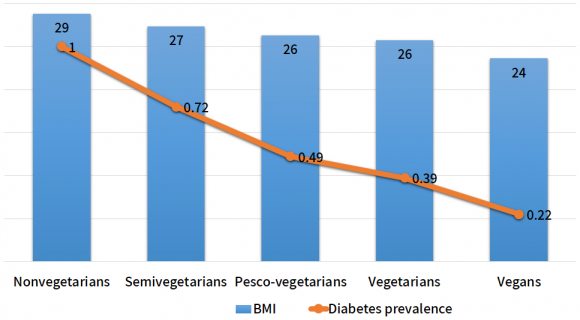
According to this research study, nonvegetarians had the highest rate of diabetes and also the highest BMI.
Check your BMI
BMI (body mass index) is a formula developed by Adolphe Quetelet in the 1850s to measure body mass.
Calculate your BMI using this formula: BMI = weight (kg) / [height (m) x height (m)]. Example for a person with a height of 176 cm and a weight of 68 kg:
1,76 m x 1,76 m = 3,0976
68:3.0976 = 21,952 (BMI 22)
BMI calculation using the English System: BMI = [weight (lb) / height (in) / height (in)] x 703. Example for a person with a height of 69.29 in and a weight of 150 pounds.
150 lb / 69.29 in / 69.29 in = 0.031
0.031 x 703 = 21.963 (BMI 22)
Although this method is widely used and allows accurate comparisons between groups, it has several disadvantages:
- It doesn’t take into consideration whether or not the weight comes from lean muscle or from fat, overestimating the risk for healthy people who are more muscular and underestimating the risk for people who are at a “normal weight” but have more body fat.
- it doesn’t indicate the place where the fat is located in the body (visceral fat, located around the organs, is more dangerous than fat located underneath the skin)
- It doesn’t take age or sex into account (women have more fat compared to men, and older people have more fat compared to younger people).
There are various alternative methods that can be used alone or in combination and have a higher level of accuracy: Body Adiposity Index, the measurement of waist circumference, Waist-to-Hip Ratio, Hydrostatic Weighing, and measuring body fat.
The spillover effect — an explanation for the relationship between obesity and diabetes
When people gain weight, it isn’t the number of fat cells that increases, but rather the size of the existing cells. The fat builds up inside, causing the cells to enlarge. At a certain point, the fat in the cells then spills into the bloodstream, generating the same impairment of "insulinsignaling" that people experience after eating a high-fat meal.
Even if an obese person is actually eating healthy, because of this spillover effect, the cells may be constantly spilling fat into the bloodstream. On the other hand, a person on a plant-based diet, even if they weigh the same as an omnivore, will have less fat trapped in their cells; better "insulinsensitivity", blood sugar, and "insulinlevels"; and an improved function of the pancreatic cells.27
6. The impact of organic pollutants on type 2 diabetes
The chemical pollutants released in the environment end up in animals’ bodies and are later ingested by humans.
The chemicals with a potent risk for diabetes are:
- Hexachlorobenzene — found in canned sardines and salmon fillets
- Polychlorinated biphenyls — found in marine, mammal, and dairy products
These toxins are then stored by humans in their own fat reservoirs, accounting for a disrupted hormonal balance, obesity, "insulinresistance", nonalcoholic fatty liver disease, and consequently, higher rates of diabetes.
7. Reducing inflammation helps control and reverse type 2 diabetes
Inflammation is a natural reaction in the human body, a way that it deals with infections and injuries.
 | It aims to repair the damaged tissue. Normally, it is a short-term reaction, but because of oxidative stress and imbalances in the immune system, it can become chronic. When the immune system comes into contact with an external factor (a pathogen or food), this triggers the release of pro-inflammatory cytokines. These cytokines can directly enhance "insulinresistance" in muscle and liver cells.30 |
Carotenoids, a class of phytonutrients (“plant chemicals”) found in red, yellow, and orange fruits and in vegetables, have been shown to reduce inflammation. Various studies have demonstrated that when a person has a higher concentration of carotenoids in their body, they have a lower risk of diabetes.31 In other words: a plant-based diet can reverse type 2 diabetes.
8. Lifestyle as a means to prevent and reverse type 2 diabetes
A sedentary lifestyle is one of the most important risk factors for type 2 diabetes. Research studies have shown that engaging in a moderate exercise program results in a reduction of diabetes markers (hemoglobin A1c) in eight weeks.32
| Type of Exercise | What Happens in the Body |
| Aerobic exercise | Muscles use glucose to function, and aerobic exercise therefore causes the level of glucose in the blood to decrease. A single session increases "insulinaction" and glucose tolerance for more than 24 hrs (up to 72 hrs). |
| Strength training | This results in lower fasting blood sugar levels 24 hrs after exercise, with greater reductions depending on the volume and intensity of the exercise |
According to the Human Movement Sciences Department at Old Dominion University, Virginia32, a combination of aerobic exercise and strength training is the most effective way to manage blood sugar levels. New "musclemass" increases the sugar uptake from the blood and its usage as fuel, whereas aerobic exercise increases "insulinaction".
Special attention should be paid when patients have other diabetes complications (e.g., circulatory disease, neuropathy, or retinopathy). Furthermore, if the blood sugar levels are not kept under control, patients can develop hyper- or hypoglycaemia during exercise. In this case, it is advisable to adjust or closely monitor medication.
Even if it might seem to be a logical and easy treatment option, an intensive blood-sugar-lowering therapy was proven to actually increase subjects’ mortality, by accelerating ageing and promoting cancer, obesity, atherosclerosis, and inflammation in the arteries.33
Despite the large number of studies on the impact of nutrition in preventing and reversing type 2 diabetes, this disease is only becoming more prevalent. Only one in three prediabetic patients reports ever being told by the doctor to exercise and improve their diets.34
Nevertheless, the World Health Organization stresses that diabetes can be treated, and its consequences avoided or delayed with diet, physical activity, medication and regular screening and treatment for complications.
Literature — sources:
34 sources
- Lempainen J, Tauriainen S, Vaarala O, Mäkelä M, Honkanen H, Marttila J, et al. Interaction of enterovirus infection and cow’s milk-based formula nutrition in type 1 diabetes-associated autoimmunity. Diabetes Metab Res Rev. 2012;28(2):177–85.
- Pratley RE. The early treatment of type 2 diabetes. Am J Med. 2013;126(9 Suppl 1):S2–9.
- Hofe CR, Feng L, Zephyr D, Stromberg AJ, Hennig B, Gaetke LM. Fruit and vegetable intake, as reflected by serum carotenoid concentrations, predicts reduced probability of PCB-associated risk for type 2 diabetes: NHANES 2003–2004. Nutr Res. 2014 Apr; 34(4): 285–293.
- Roden M, Price TB, Perseghin G, Petersen KF, Rothman DL, Cline GW, et al. Mechanism of free fatty acid-induced "insulinresistance" in humans. J Clin Invest. 1996;97(12):2859–65.
- Roden M, Krssak M, Stingl H, Gruber S, Hofer A, Fürnsinn C, et al. Rapid impairment of skeletal muscle glucose transport/phosphorylation by free fatty acids in humans. Diabetes. 1999;48(2):358–64.
- Santomauro AT, Boden G, Silva ME, Rocha DM, Santos RF, Ursich MJ, et al. Overnight lowering of free fatty acids with Acipimox improves "insulinresistance" and glucose tolerance in obese diabetic and nondiabetic subjects. Diabetes. 1999;48(9):1836–41.
- Krssak M, Falk Petersen K, Dresner A, DiPietro L, Vogel SM, Rothman DL et al. Intramyocellular lipid concentrations are correlated with "insulinsensitivity" in humans: a 1H NMR spectroscopy study. Diabetologia. 1999;42(1):113–6.
- Vergnaud AC, Norat T, Romaguera D, Mouw T, May AM, Travier N, et al. Meat consumption and prospective weight change in participants of the EPIC-PANACEA study. Am J Clin Nutr. 2010;92(2):398–407.
- Mollard RC, Luhovyy BL, Panahi S, Nunez M, Hanley A, Anderson GH. Regular consumption of pulses for 8 weeks reduces metabolic syndrome risk factors in overweight and obese adults. Br J Nutr. 2012;108 Suppl 1:S111–22.
- Clement, B. Food Is Medicine. The Scientific Evidence. Summertown, Hippocrates Publications; 2012.
- Mbikay M. Therapeutic potential of Moringa oleifera leaves in chronic hyperglycemia and dyslipidemia: a review. Front. Pharmacol., 01 March 2012.
- Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ. Cinnamon Use in Type 2 Diabetes: An Updated Systematic Review and Meta-Analysis. Annals of Family Medicine. 2013;11(5):452-459.
- Satija A, Bhupathiraju SN, Rimm EB, Spiegelman D, Chiuve SE, Borgi L et al. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. Moore SC, ed. PLoS Medicine. 2016.
- Kahleova H, Hrachovinova T, Hill M, et al. Vegetarian diet in type 2 diabetes—improvement in quality of life, mood and eating behaviour. Diabet Med. 2013;30(1):127–9.
- Anderson JW, Ward K. High-carbohydrate, high-fiber diets for "insulintreated" men with diabetes mellitus. Am J Clin Nutr. 1979;32(11):2312–21.
- Liese AD, Weis KE, Schulz M, Tooze JA. Food Intake Patterns Associated With Incident Type 2 Diabetes: The "InsulinResistance" Atherosclerosis Study .Diabetes Care. 2009;32(2):263-268. (EE: Olivenöl esetzt durch "Nüsse und Samen mit gutem LA:ALA-Verhältnis").
- Hyman M. The Blood Sugar Solution. New York, Hyman Entreprises, 2012
- Pasin G, Comerford KB. Dairy Foods and Dairy Proteins in the Management of Type 2 Diabetes: A Systematic Review of the Clinical Evidence. Advances in Nutrition. 2015;6(3):245-259.
- McGregor RA , Poppitt SD . Milk protein for improved metabolic health: a review of the evidence. Nutr Metab (Lond) 2013;10:46.
- Liu S, Choi HK, Ford E, Song Y, Klevak A, Buring JE et all. A Prospective Study of Dairy Intake and the Risk of Type 2 Diabetes in Women. Diabetes Care 2006 Jul; 29(7): 1579-1584.
- Tong X , Dong JY , Wu ZW , Li W , Qin LQ . Dairy consumption and risk of type 2 diabetes mellitus: a meta-analysis of cohort studies. Eur J Clin Nutr 2011;65:1027–31.
- Gao D , Ning N , Wang CX , Wang YH , Li Q , Meng Z , Liu Y , Li Q . Dairy Products Consumption and Risk of Type 2 Diabetes: Systematic Review and Dose-Response Meta-Analysis. PLoS ONE 2013.
- Aune D , Norat T , Romundstad P , Vatten LJ . Dairy products and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Am J Clin Nutr 2013;98:1066–83.
- Hannon TS, Rao G, Arslanian SA. Childhood obesity and type 2 diabetes mellitus. Pediatrics. 2005;116(2):473–80.
- Sabaté J, Wien M. Vegetarian diets and childhood obesity prevention. Am J Clin Nutr. 2010;91(5):1525S–1529S.
- Tonstad S, Butler T, Yan R, Fraser GE. Type of vegetarian diet, body weight, and prevalence of type 2 diabetes. Diabetes Care. 2009;32(5):791–6.
- Goff LM, Bell JD, So PW, Dornhorst A, Frost GS. Veganism and its relationship with "insulinresistance" and intramyocellular lipid. Eur J Clin Nutr. 2005;59(2):291–8.
- Magliano DJ, Loh VHY, Harding JL, Botton J, Shaw JE. Persistent organic pollutants and diabetes: a review of the epidemiological evidence. Diabetes Metab. 2014;40(1):1–14.
- ATSDR (Agency for Toxic Substances and Disease Registry)Toxicological Profiles. Atlanta, GA: ATSDR; 2000. [Accessed March 27, 2011]. Toxicological Profile for Polychlorinated Biphenyls (PCBs) www.atsdr.cdc.gov /ToxProfiles /tp17.pdf.
- Badawi A, Klip A, Haddad P, Cole DEC, Bailo BG, El-Sohemy A, Karmali M. Type 2 diabetes mellitus and inflammation: Prospects for biomarkers of risk and nutritional intervention. Diabetes Metab Syndr Obes. 2010; 3: 173–186.
- Hofe CR, Feng L, Zephyr D, Stromberg AJ, Hennig B, Gaetke LM. Fruit and vegetable intake, as reflected by serum carotenoid concentrations, predicts reduced probability of PCB-associated risk for type 2 diabetes: NHANES 2003–2004. Nutrition research (New York, NY). 2014;34(4):285-293.
- Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR et al. Exercise and Type 2 Diabetes: The American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147-e167.
- The Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
- Karve A, Hayward RA. Prevalence, diagnosis, and treatment of impaired fasting glucose and impaired glucose tolerance in nondiabetic U.S. adults. Diabetes Care. 2010;33(11):2355–9.


Comments